Living in a post antibiotic world…a reality I would rather not experience – Part 3
This is part 3 of a 3 part blog on antimicrobial resistance. In this final instalment I am expanding on the primer presented in Part 1.
Part 1 – 5 Easy Things You Can Do To Reduce Antimicrobial Resistance and a primer on the issue of antimicrobial resistance
Part 2 – Alternatives to Medicinal Antimicrobial Use
Part 3- Antimicrobial Resistance – The Science Stuff
I am again starting with the good news. After the good news I am going to really geek-out and talk about the research and science around antimicrobial resistance. At the end of this blog I have included a list of some resources that will give you lots more information about antimicrobial resistance.
The Good News...
There are things we can do - 5 Easy Things You can do to Reduce Antimicrobial Resistance
There are Alternatives to Medicinal Antimicrobial Use
The Best News…
Using fewer antimicrobials may effectively eliminate antimicrobial resistant ‘superbug’ populations!
Microbes compete with each other for resources. Studies suggest that carting around antimicrobial resistance is hard work and superbugs require more resources to reproduce – in more scientific terms, there is a fitness cost associated with antimicrobial resistance. Paying the fitness cost of antimicrobial resistance makes evolutionary sense as long as there is a selective pressure to do so - i.e. antimicrobials keep killing your competition and clearing the way for your offspring. Eliminating the selective pressure to have antimicrobial resistance (eliminating the use of antimicrobials) will put superbugs at a competitive disadvantage since they require more resources to produce offspring. In the absence of antimicrobials superbugs will have to either drop their antimicrobial resistance or be overtaken by the competition.
Who is affected?
Everyone. Antimicrobial resistance is a global issue that affects people from all walks of life, but is of particular significance for the young, the elderly and anyone who is immune compromised, e.g. chemotherapy patients, people with immune disorders, people battling chronic illnesses, etc.
Antimicrobials (antibiotics, antivirals, antiparasitics, and antifungals) are the cornerstone of modern medicine. Superbugs, in addition to hobbling modern medicine’s ability to fight routine infectious disease, make many other routine treatments very risky. Many of the surgical procedures that have become common place – i.e. joint replacements, cardiac by-pass, organ transplants, etc. – become very risky without antibiotics to fight post surgical infections. Modern medicine’s treatment of many chronic diseases such as diabetes, asthma, rheumatoid arthritis and cancer weaken your immune system. These treatments rely on antibiotics to fight the inevitable subsequent infections that result. As stated in the CDC report Antibiotic Resistance Threats in the United States, 2013 if the ability to use antimicrobials to fight infections is lost “…the ability to safely offer people many of the life-saving and life-improving modern medical advances will be lost with it.”
What is going on?
Pathogenic microbes (bacteria, parasites, viruses and fungi) are developing resistance to all of our antimicrobial agents (antibiotics, antivirals, antiparasitics, and antifungals). These ‘superbugs’ are evolving faster than we are developing new antimicrobial agents to kill them. As a result simple infections – like bladder, ear, and candidiasis infections - are increasingly resistant to antimicrobial treatments and posing serious health concerns.
Some researchers note that the development of new antimicrobials is not as profitable as the development of other drugs. They cite the lack impetus on the part of the pharmaceutical industry to develop new antimicrobials as one of the major hurdles in the fight against superbugs. Other researchers note that it is the rapid development and spread of resistance to new antimicrobials – limiting the effective use of the new antimicrobial – that makes new antimicrobial development unprofitable.
Is this happening now?
Yes. The World Health Organization is predicting that a ‘post antibiotic world’ is a very real possibility during this century. Today, health care workers are encountering an increasing number of antibiotic resistant infections.
In 2013 the CDC reported that superbug infections directly resulted in the death of at least 23,000 people in the USA and that numerous others died from other conditions that were complicated by an antibiotic-resistant infection.
In its Antibiotic Resistance Threats in the United States, 2013 report the CDC has identified and ranked various microbes based on the threat level they pose to the general population. Microbial strains that have been identified as Urgent include clostridium difficile (C. difficile), salmonella, e-coli, and shigella. Twelve microbes have been identified as Serious and they include strains of: campylobacter and salmonella, common causes of food poisoning; candida, a fungus that causes genital yeast infections, cradle cap, and thrush; staphylococcus aureus (MRSA) which causes a range of illnesses, from skin and wound infections to pneumonia and bloodstream infections; and, tuberculosis (TB).
Where are the 'superbugs'?
Antimicrobial resistant ‘superbugs’ used to be mainly confined to hospital environments where antimicrobial use was high and many pathogens were prevalent. Sadly this is no longer the case and superbugs have spread into the community and our homes.
It makes sense that the emergence of superbugs was initially detected in hospitals: if someone is unresponsive to antibiotics and getting worse they are admitted to the hospital, along with the superbugs they are carrying; the superbugs are now in the hospital and able to easily infect patients with already compromised immune systems. The Globe and Mail has reported that in Canadian hospitals 1 out of 12 patients is colonized or infected by a superbug.
More alarmingly, researchers have discovered a trend of superbug proliferation in the general community. Non–healthcare related infections with superbugs like Methicillin-resistant Staphylococcus aureus (MRSA), that causes a range of illness from skin and wound infections to pneumonia and bloodstream infections, have rapidly increased.
Why is this happening?
We are overusing and misusing antimicrobial agents - from the antimicrobial/bacterial soaps, cleaners and spays we use around our homes to the broad spectrum antibiotics used prophylactically and as growth promoters in our livestock industries.
The overuse and misuse of antibiotics creates a selective pressure for antimicrobial resistance - susceptible microbes are eliminated while resistant microbes are left to flourish with no competition. At first this may only be a very small percentage of the original population, but over time the majority of microbes will be antimicrobial resistant.
Research identifies 3 likely reasons for the rapid spread of superbugs in the general population: household use of antimicrobials, non-therapeutic use of antimicrobials in the livestock industry, and medical misuse of antimicrobials.
1. Household use of antimicrobials
The use of antimicrobials in our homes has rapidly increased, particularly triclosan, and with it the populations of antimicrobial resistant microbes in our homes have also increased. The antimicrobials marketed for household use are either the same, or very similar to the antimicrobials used medically. The more we use household antimicrobials the greater the chance that we are inadvertently breeding the antimicrobial resistant microbes that are threatening our health.
2. The overuse and misuse of antibiotics in the livestock industry.
Many years ago the livestock industry realized that the use of antibiotics increased the growth rate and decreased the nutrient requirements of animals. Today the majority of antibiotic use in North America is for non-therapeutic use in the livestock industry. The blanket application of antibiotics creates an overwhelming selective pressure for antibiotic resistance. The antibiotic resistant microbes from the livestock industry are transmitted directly to us via our food supply or indirectly via environmental contamination from sewage and water outflows from the feedlots.
3. Medical misuse
As noted above every time an antimicrobial is used it creates a selective pressure that favors antimicrobial resistant microbes. The misuse of both prescription and over-the-counter antimicrobials (e.g. Polysporin) prophylactically, as a first resort (versus a last resort), or in a broad spectrum format (non-specific to the infection) is adding to the problem. Also adding to the problem is misuse of properly prescribed antibiotics (incomplete dosing, sharing, etc.) creating ideal environments for the proliferation antibiotic resistance.
How are 'superbugs' spreading so fast?
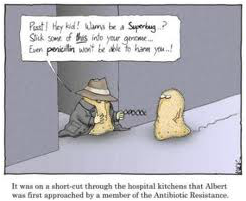
Every time we misuse an antimicrobial we are breeding ‘superbugs’. To make matters worse ‘superbugs’ are generous and they share their antimicrobial resistance with other pathogens – even other species of pathogens.
As noted above every time we use an antimicrobial we are creating a competitive advantage for microbes that are antimicrobial resistant. Microbial populations can be intrinsically resistant to an antimicrobial – they are insensitive to a particular antimicrobial due to inherent structural or functional characteristics. This fact alone doesn’t fully explain: why there are now so many resistant stains of microbes; why so many strains are resistant to numerous antimicrobials; and, how resistance to even new and very powerful antimicrobials is spreading so fast.
It turns out that microbes are able to acquire resistance to antimicrobial agents that they were previously susceptible to. Acquired resistance can result from the mutation of genes and from the acquisition of foreign resistance genes from other microbes. Microbes will transfer resistance to other members of the same microbial species, as well as to microbes in another genus or species. In this way multiple drug resistance can be accumulated and passed on.
You can geek out too - Learn More
Antimicrobial resistance: global report on surveillance 2014
Antibiotic resistance threats in the United States, 2013
Antimicrobial Resistance Learning Site
Evidence of Extensive Interspecies Transfer of Integron-Mediated Antimicrobial Resistance Genes among Multidrug-Resistant Enterobacteriaceae in a Clinical Setting
The antimicrobial resistance crisis: causes, consequences, and management
Antibiotic resistance mechanisms of clinically important bacteria.
Mechanisms of Antimicrobial Resistance in Bacteria
Bacterial Resistance to Antibiotics
Antibiotic Awareness
Antibiotic resistance and its cost: is it possible to reverse resistance?
Insights into Antibiotic Resistance Through Metagenomic Approaches
Food, Farm Animals and Drugs
Health Canada tightens antibiotic use
Phasing Out Certain Antibiotic Use in Farm Animals
A Ticking Time Bomb: Eliminating Antibiotic Overuse in Animal Agriculture
Hospital cleaning in the 21st century
Antibacterial cleaning and hygiene products as an emerging risk factor for antibiotic resistance in the community
Antimicrobial Resistance In Hospitals
How hospitals are on the front lines in a new era of germ warfare How hospitals are on the front lines in a new era of germ warfare
Should antibacterial soap be outlawed?
Triclosan and antimicrobial resistance in bacteria: an overview.
Triclosan and Antibiotics resistance
Antibiotics and antibiotic resistance in water environments
Flying the coop: Antibiotic resistance spreads to birds, other wildlife
Something to remember: Healthy bodies have strong immune systems that can fend off pathogens naturally – without the use of antimicrobials. And, each time your body successfully fights an infection it learns and fending off subsequent pathogens becomes easier. Nutrition and homeopathic support can help naturally restore and maintain health.

 RSS Feed
RSS Feed
